Medical conditionChronic Pain
introductionIn 1990 I qualified as a doctor. In 2015 I became a patient. I developed thoracic outlet syndrome in both arms. My world changed overnight. My life as a busy GP, educator, mum, wife and friend came to a crashing halt and I swapped my prescription pad and doctor’s bag for a bottle of pregabalin and a fistful of hospital appointments. My acute nerve compression progressed into chronic pain and with this the awareness of how little my 25-year medical career had taught me about managing chronic pain.
Key insightsChronic pain is an invisible illness affecting around 8 million adults in the UK.
It is often difficult to treat, and interventions don’t always relieve suffering.
The secondary effects - such as fatigue, anxiety, loneliness, and low self-esteem - can be just as disabling as the pain itself.
General OverviewChronic pain is an invisible illness that affects around 8 million adults in the UK. Unlike acute pain, which signals injury or illness and typically resolves, chronic pain can persist for months or years and is now recognised as a condition in its own right. It is often difficult for patients to describe and for clinicians to fully understand, and treatments are not always straightforward. In addition to the pain itself, many people live with its secondary effects - such as fatigue, anxiety, loss of sleep, loneliness, and reduced self-esteem - which can have just as great an impact on daily life. Increasingly, a biopsychosocial approach is used to understand and manage chronic pain, recognising the interaction between physical, psychological, and social factors and focusing on improving quality of life rather than searching for a single cause or cure.
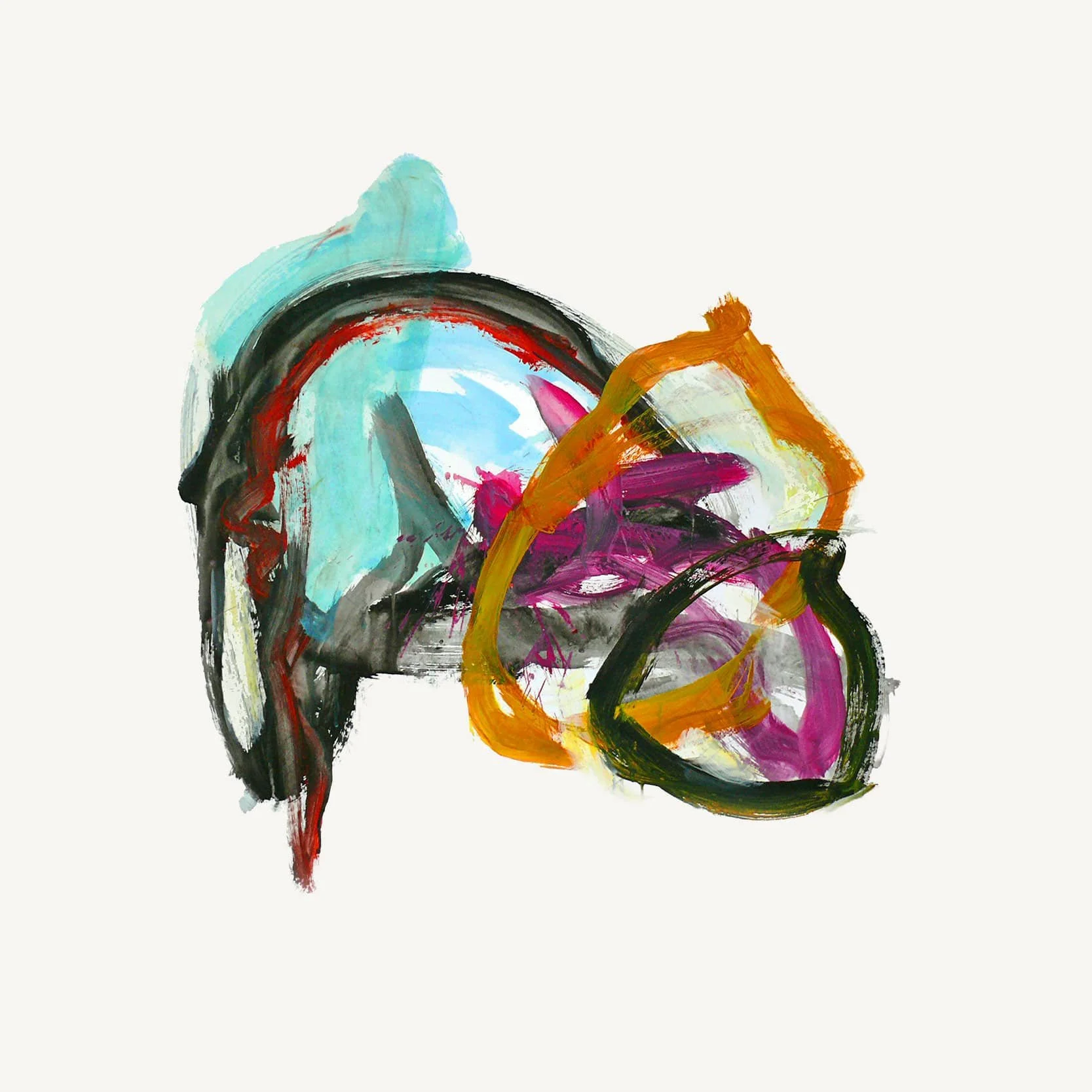
Art ResourcesArt offers a way to express and explore the experience of pain when words fall short. These works invite reflection, discussion, and new perspectives on what it means to live with chronic pain.
-
Reproduced under Creative Commons license
Possibly the most well-recognised painting associated with chronic pain is Frida Kahlo’s ‘A Broken Column’. She painted this picture just after she had spinal surgery to correct the consequences of a life-changing traffic accident.
In what way does Frida convey her pain and suffering in this picture?
A Broken Column
Frida Kahlo
1944
Reproduced under Creative Commons license.
Possibly the most well-recognised painting associated with chronic pain is Frida Kahlo’s ‘A Broken Column’. She painted this picture just after she had spinal surgery to correct the consequences of a life-changing traffic accident.
In what way does Frida convey her pain and suffering in this picture?
The Wounded Deer
Frida Kahlo
1946
Reproduced under Fairuse. This is another of Frida’s paintings.
Maybe she sees a similarity between her own struggle with pain and that of the deer’s constant struggle to survive being hunted? What do you think?
-
Reproduced under Creative Commons license
Possibly the most well-recognised painting associated with chronic pain is Frida Kahlo’s ‘A Broken Column’. She painted this picture just after she had spinal surgery to correct the consequences of a life-changing traffic accident.
In what way does Frida convey her pain and suffering in this picture?
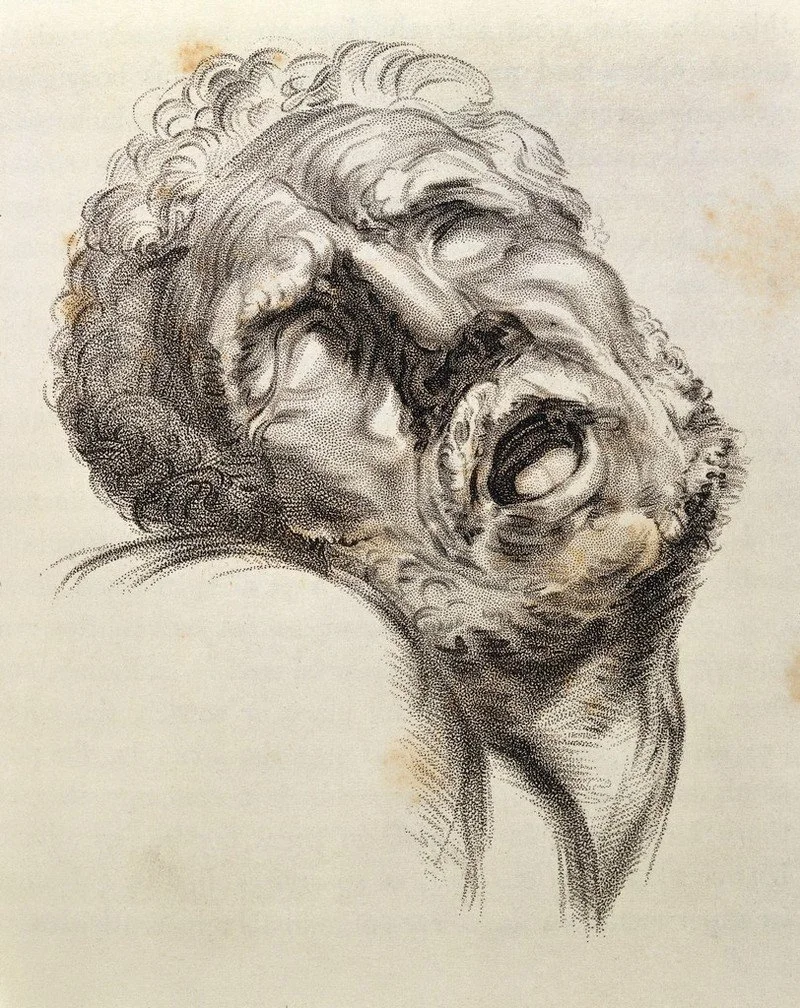
Pain
Sir Charles Bell
Welcome Collection. Reproduced under Creative Commons licence.
Charles Bell was a doctor who spent much of his life drawing with the aim of capturing the ‘expression of emotion related to illness and disease’. This is his representation of ‘pain’ published in his book ‘The anatomy and philosophy of expression as connected with the fine arts’ (London, 1844), p. 157.
What picture or image would you choose to represent chronic pain?
1844
Pain like ice
Deborah Padfield
2001-2006
Deborah Padfield is an artist who suffers from chronic pain. After a conversation with her consultant, she decided to use her art to express how her pain felt to her doctors. This resulted in two projects INPUT and Face2face in which she worked with chronic pain patients to create visual representations of how their pain felt and what it meant to them. With their permission and support, these photographic images were made into ‘pain cards’ to be used by doctors in pain clinics to communicate with their chronic pain patients.
Chronic pain has inspired powerful reflections in literature, from personal memoirs to cultural analysis. These works prompt thought and discussion about what it means to live with ongoing pain.
Resource library - Books & Literature -
On Being Ill (essay)
by Virginia Woolf
Woolf observed how illness resists language: “Even a schoolgirl in love has Shakespeare and Keats to speak her mind for her; but let a sufferer try to describe a pain to a doctor and language at once runs dry.”
-
How Much Pain Is Too Much Pain
by Hilary Mantel
A short story reflecting Mantel’s own experiences of chronic pain. She describes a consultation where, for the first time, she felt her pain was truly listened to — an encounter that was “therapeutic” in itself.
-
The Language of Pain
by David Biro (2010)
Explores how pain is invisible and often doubted by doctors, friends, and family. Biro suggests that what makes pain most painful is the inability to express it to others.
-
The Land of Pain
by Alphonse Daudet
Daudet’s journal of incurable pain contains vivid reflections:“Pain has a life of its own.”
“It’s bearable, and yet I cannot bear it.”
“Pain is always new to the sufferer, but it loses its originality for those around him.”
prompt Now it’s your turn…
Can you find a poem to help you understand chronic pain?
Can you write a poem about what it feels like to manage a patient in pain?
My own thoughts & POEMSTo help me manage my chronic pain, I was fortunate to attend the residential pain management course at the Walton Centre in Liverpool. It was a revelation to learn psychological strategies for managing chronic pain in a group with other patients.
Like many people in the group I found being creative helped me make sense of my new world and cope with the sudden onset of a life changing illness.
A visual metaphor used by the Pain Management Team at The Walton Centre in Liverpool
I wrote the next three poems after several frustrating visits to hospital outpatients where none of the consultants I saw seemed to believe I had a problem because my symptoms did not fit neatly with their list of possible diagnosis. (August 2015)
The tranquillity of my garden and the ability to slip back into things I loved as a child enabled me to maintain my sense of wellbeing despite the pain and fatigue. (May 2015)
In My Garden
A.A. Milne
Halfway down the stairs is a stair where I sit. There isn’t any other place quite like it.
I rock gently in my hammock. Sunlight shines through the cherry tree leaves, making patterns on my face and arms.
My hand reaches out, touching the cool of the fossilised wood. I rock back and forth- at one with the world- the earth and nature.
A spider dances across the dark slate then disappears into the bank of ferns. I am hidden from view. Hidden or hiding from my real world.
All sorts of funny thoughts run through my head. It isn’t really anywhere, it’s somewhere else instead.
The transition from a ‘highly functioning’ adult with many roles to patient was very challenging. (Oct 2015)
After a time off work with the support of amazing colleagues and the flexibility of my post I returned to work as a GP Training Programme Director. The statement ‘not all disabilities are visible’ helped me struggle back to work looking well but not feeling it. (Sept 2017)
This is something I did not previously understand. (March 2017)
The line of illness
by Nicola Gill (me)
March 2017
The line is invisible
to doctors
who think
they understand
the pain
the fatigue
the loss of identity
that is illness
The line is a border.
Patients have no visa no passport to cross back to the other side that is health.
The pain is ongoing, the care has improved, my wellbeing is good.
These poems have helped me make sense of my new world.
Medical resourcesChronic pain is complex, and new evidence shows it can be explained through a biopsychosocial approach. This should have resulted in a change in how clinicians talk to patients and the interventions they offer to help people live well with pain. However, many patients and clinicians still focus on identifying a single cause and treatment so there is more that can be done to use the evidence in patient care and education.
These are two excellent medical resources:
page updated september 2025